What is lipodystrophy?
Lipodystrophy syndromes are extremely rare disorders. However, the core characteristic is complete (generalised) or partial absence of subcutaneous adipose tissue or unusual fat distribution. The loss of adipose tissue is frequently associated with serious metabolic complications and leptin deficiency. All lipodystrophy subtypes can be associated with insulin resistance, altered glucose tolerance or diabetes, and hypertriglyceridemia leading to a risk of acute pancreatitis and organ damage.
Pathophysiology of lipodystrophy
Lipodystrophies can be characterised by the extent of the adipose tissue loss, generalised loss over the whole body or partial loss. They are also classified into whether they are inherited (congenital or familial) or acquired. This leads to four main types: congenital generalised lipodystrophy (CGL), acquired generalised lipodystrophy (AGL), familial partial lipodystrophy (FPLD) and acquired partial lipodystrophy (APL). In all subtypes, adipose tissue is dramatically reduced leading to numerous metabolic complications. Adipose tissue is important as an energy store, in maintaining energy homeostasis and secreting hormones such as leptin. A significant loss of adipose tissue can result in significant metabolic disruption and leptin deficiency.
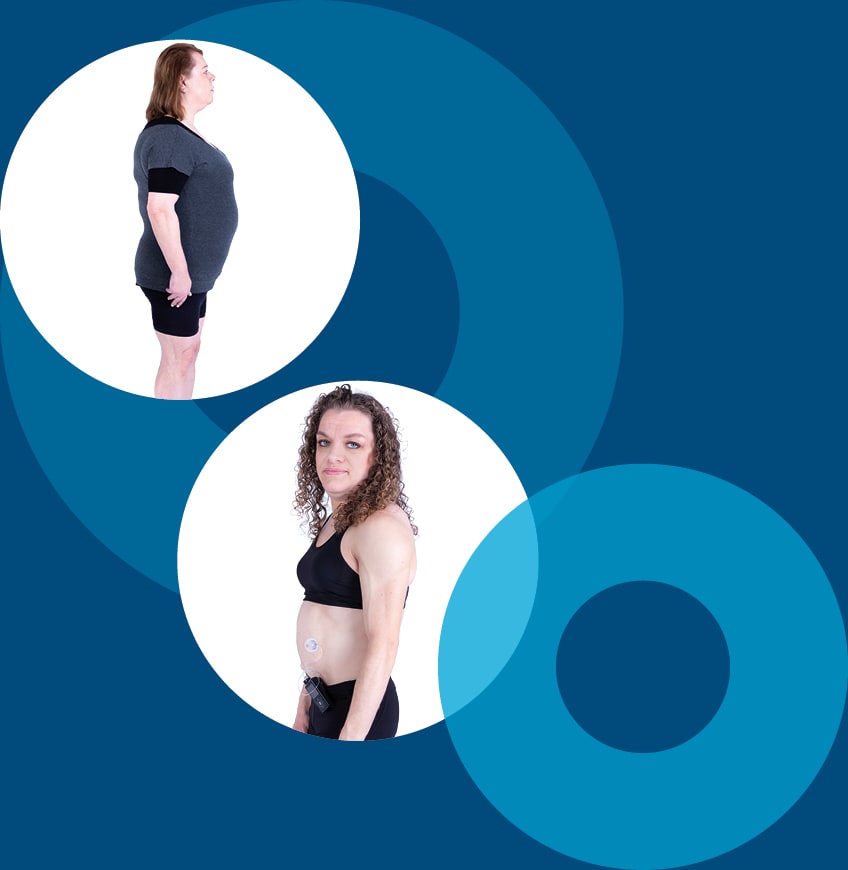
Generalised and partial lipodystrophy are always connected to a lack of subcutaneous adipose tissue. The extent and location of adipose tissue loss depends on the subtype of lipodystrophy.
How is leptin related to lipodystrophy?
Adipocytes have an endocrine function and secrete hormones (adipokines), including leptin. Leptin is an adipocyte-secreted hormone that regulates energy homeostasis as well as metabolic, reproductive, neuroendocrine, and immune functions. Normally, excess energy and fat is stored in adipose tissue. In lipodystrophy, adipose tissue is markedly reduced leading to leptin deficiency and adipose storage capacity is exceeded. Combined, these can cause ectopic fat deposition and metabolic complications.
When fat storage capacity is exceeded, the excess energy is stored ectopically.
Because little or no subcutaneous adipose tissue is present in partial lipodystrophy (PL) and generalised lipodystrophy (GL), storage increasingly takes place in any remaining body adipose tissue or ectopically in the liver, heart, kidneys, pancreas and muscles. A leptin deficiency caused by the loss of adipose tissue makes a significant contribution to the metabolic complications seen in lipodystrophy patients and also leads, in particular, to insatiable hunger and excess food intake, which exacerbates the metabolic comorbidities further.
Clinical consequences of leptin deficiency
Adipose tissue loss and accompanying leptin deficiency can lead to complex clinical outcomes such as insulin resistance with hard to treat diabetes mellitus (possibly with acanthosis nigricans), Polycystic Ovary Syndrome (PCOS), hypertriglyceridaemia, fatigue, muscular pain and insatiable hunger (hyperphagia).

Insulin resistance
Patients with generalised and partial lipodystrophy exhibit diabetes with a high insulin dose requirement
- ≥ 200 U/day, ≥ 2 U/kg/day
- Use of U-500 insulin
Hyperphagia
Insatiable hunger and hyperphagia caused by leptin deficiency can lead to an increased intake of calories, which in turn can result in deterioration of the metabolic state and increased ectopic fat storage.
Ectopic fat deposition
Lipodystrophy patients are heterogenous in appearance. There may be fat accumulation where adipose tissue remains and ectopic fat deposition in muscles and internal organs such as the liver, kidneys and heart
Hypertriglyceridaemia
Severe hypertriglyceridaemia:
- ≥ 5.65 mmol/L (≥ 500 mg/dL)
- ≥ 2.83 mmol/L (≥ 250 mg/dL) despite treatment and diet
- History of pancreatitis associated with hypertriglyceridaemia
Leptin deficiency may lead to a complex pathology and severe clinical consequences.
C-LD/UK/0089
Date of preparation October 2023